Abstract
Introduction: Hematopoietic cell transplantation (HCT) carries significant risks for mortality, which are not proportionally shared across individuals. Among HCT recipients, we have previously shown that low socioeconomic status (SES) is predictive of increased mortality following HCT, and the underlying mechanism for this outcome is not fully explained by race, insurance status or access to care. Furthermore, following HCT, the donor immune system replaces that of the recipient, leading to long-term engraftment with donor-derived immune cells. Previous work has not addressed the influence of donor socioeconomic factors on HCT recipient outcomes. Therefore, we hypothesized that SES would impact donor hematopoietic cells and this effect would be transferrable and associated with adverse recipient outcomes.
Methods: Recipients of matched unrelated donor allogeneic peripheral blood stem cell HCT between 2000-2013 for hematologic malignancy, resided in the United States (US) with a documented ZIP code, and had a HCT donor with documented US ZIP code were identified from the Center for International Blood and Marrow Transplantation Research (CIBMTR). Using donor ZIP code, SES measures of household income, poverty, education, housing and employment were derived from the U.S. Census American Community Survey. A standardized donor SES composite score was computed as an equally weighted average of the 5 standardized SES variables (mean composite score = 0, standard deviation (SD) = 1). Multivariable models, adjusted for donor and recipient characteristics, were used to evaluate associations between donor SES composite score with HCT recipient disease free survival (DFS), overall survival (OS), treatment related mortality (TRM), relapse, and acute and chronic graft versus host disease (GVHD). Results were considered significant if P < 0.01.
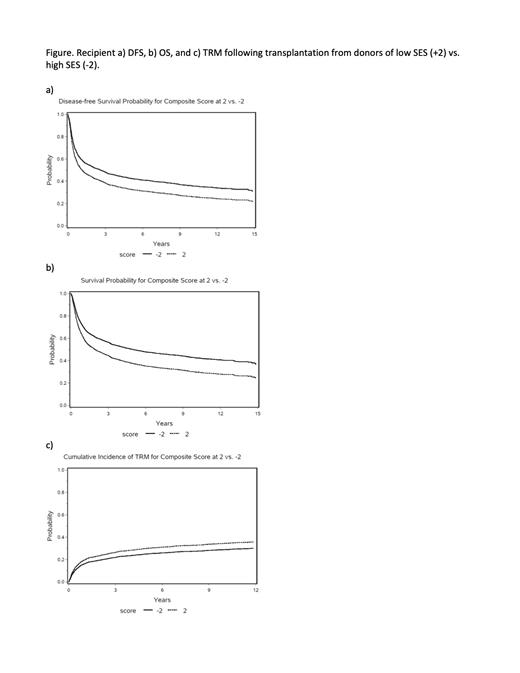
Results: Among 2,005 HCT recipients, median age at diagnosis was 51 years (range 1-77), 44% were female, and 55% had acute myeloid leukemia. Median post-HCT follow up was 120 months (range 4-219). Donors were 44% female and median age at hematopoietic cell donation was 34.7 years (range 18-62). The standardized donor composite scores ranged from -2.6 to 3.9, with a higher composite score indicative of greater socioeconomic disadvantage. Multivariable analyses identified significant associations between the standardized donor SES composite score and DFS (HR 1.07 per SD SES, 95% CI 1.02-1.13; p=0.0088), OS (HR 1.09 per SD SES, 95% CI 1.04-1.15; p=0.0007), and TRM (HR 1.10 per SD SES, 95% CI 1.03-1.17; p=0.0049). Significant associations were not identified between donor SES and relapse or GVHD. Quantitatively, recipients transplanted with cells from a donor of greater socioeconomic disadvantage (i.e. SES composite score 2 SD above the mean) experienced a 10% reduction in DFS and OS, and a 5% increase in TRM at 3 years compared with those transplanted with cells from a high-SES donor (SES composite score 2 SD below the mean) (Figure).
Conclusions: For the first time, we have demonstrated that socioeconomic disadvantage among HCT donors results in adverse transplant outcomes in the HCT recipient. This novel finding suggests that SES has biologic impacts down to the stem cell level that persist even when transplanted into a new host during HCT. The implications of these findings are broad and suggest the need for public health interventions targeting socioeconomic support as a means for preventing social disparities in cancer treatment outcomes.
Verneris: Novartis: Other: advisory board; jazz: Other: advisory board; Fate Therapeutics: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal